Approximately 40,000 women will die from breast cancer this year.
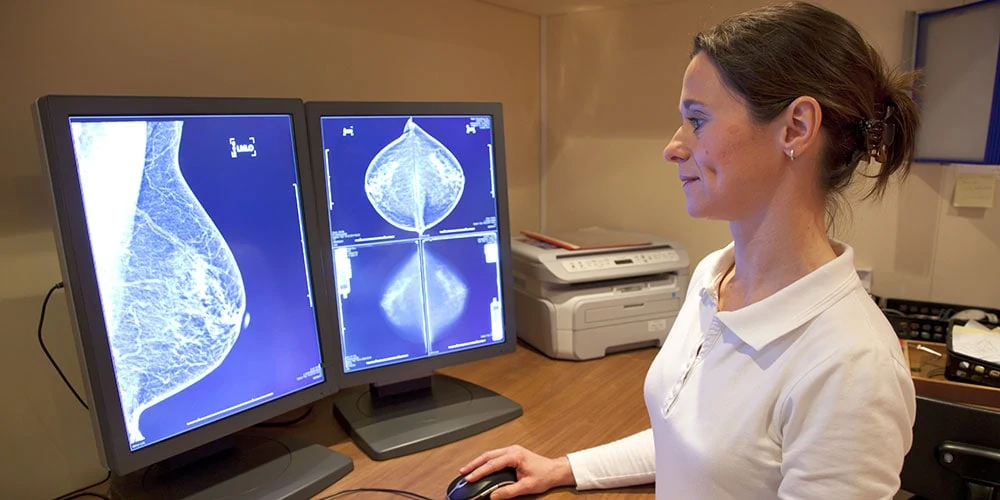
Nearly 40 million screening mammograms are administered in the United States each year. The newest generation of digital mammograms, taken with computed tomography (CT), are far advanced from yesterday’s X-ray.
Thanks to improved breast imaging technology and advancing medical expertise, hundreds of thousands of lives have been saved through the early detection of breast cancer provided by mammograms.
Approximately 300,000 women will die from heart disease this year.
Accumulating studies are now showing that, in addition to helping doctors and patients battle breast cancer, mammograms may also significantly help in the fight against women’s heart disease.
Incidentally, we should probably apologize in advance for what may seem to be an inordinate abundance of acronyms later in this article. As you will soon see, it’s hard to avoid.
What does BAC stand for?
We’ll start the acronym spree with BAC, which stands for breast arterial calcifications. These are small calcium deposits that form inside arteries within the breast tissue. The deposits run lengthwise along the inside wall of an artery. They resemble miniature railroad tracks: two parallel lines connected by cross-ties.
BACs are quite common. About 10% of women in the menopause age range have them. The incidence increases with age; about 50% of women in their 80s have BACs.
The formation of these breast calcifications has nothing to do with the calcium that a patient might ingest, whether in meals or in calcium supplements.
BACs appear as white markings on mammograms. The minerals in many deodorants can mimic the appearance of BACs. That’s why imaging technicians insist that all deodorant is removed before beginning imaging.
What causes calcification in breast tissue?
- Past injuries to, or infections in, a breast
- Breast cysts
- Past breast radiation therapy
- Family history of breast cancer
- Past surgeries
- Calcium accumulation in breast blood vessels. This is the same process that causes calcium and cholesterol to build up in blood vessels throughout the body. These deposits lead to a condition called atherosclerosis, better known as hardening of the arteries.
There are two types of breast calcifications: microcalcifications and macrocalcifications
In reading a mammogram, care must be taken to avoid confusion between calcification and fat necrosis, a lesion in the breast that can mimic the appearance of a calcium deposit.
What do microcalcifications look like?
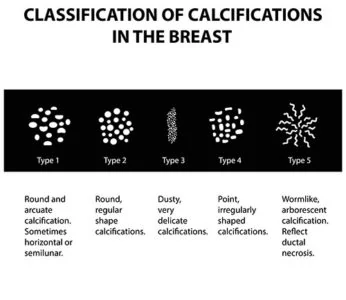
The presence of precancerous cells in suspicious calcifications may be revealed when magnification shows white specks forming discernible patterns, made up of rod-like lines.
Microcalcifications can be a marker for invasive ductal carcinoma, the type of breast cancer that accounts for about 80% of cases.
Any indications of malignancy are noted by the reporting radiologist for follow-up and further testing, such as a needle biopsy or a more invasive breast biopsy.
What do macrocalcifications look like?
Macrocalcifications appear on a mammogram as larger white spots, popcorn-like and with no noticeable pattern. They are usually noncancerous.
What are BI-RADS?
Radiology practitioners use a reporting protocol known as BI-RADS, which stands for “Breast imaging-reporting and data system.” A BI-RADS report is stratified into seven categories, ranging from category 0, “incomplete,” to category 6 “known biopsy-proven malignancy.”
Mammograms are generally understood to be all about and only about breast cancer. So it is unlikely that, under the current system, even pronounced evidence of severe microcalcification would merit a mention on a BI-RADS report.
Breast calcifications and heart disease may be related
As noted above, the calcification process that leads to BACs is similar to the process that causes atherosclerosis throughout the vascular system. Atherosclerosis isn’t a good thing anywhere, but it is particularly problematic when it causes coronary artery disease (CAD).
Coronary artery disease can arrive in the form of coronary artery calcification (CAC) or coronary artery ectasia (CAE), which occurs when a coronary artery has swollen to at least 1.5 times its usual diameter.
Information leading to early detection of heart disease is welcome
Cardiologists are well aware of most of the risk factors currently linked to heart disease. But any new source of information that might lead to early detection of impending heart problems is, of course, welcome.
This is the sort of knowledge that can enable preventative treatment. It is far better to prevent cardiac harm before it happens, rather than try to repair already incurred heart damage.
What is heart failure?
Heart failure is what happens when the heart is weakened and can’t effectively do its job of pumping blood throughout the body. Sooner or later, a weakened heart just gives up.
How mammograms can reveal a sign of heart problems
In 2019, researchers from the University of California San Diego presented preliminary research regarding the use of mammographic revelations of BAC to discover existing or impending heart failure.
The UCSD team focused on 278 middle-aged and older women. Even after accounting for other risk factors, the women with marked calcium buildup in their breast arteries had a 2.2 times greater chance of developing heart failure.
The UCSD results largely confirm a study presented at the American College of Cardiology in 2016. The American College of Cardiology study showed, for the first time, a link between the amount of calcium in the arteries of the breast, as revealed by mammography, and the level of calcium buildup in the coronary arteries.
So a mammogram that shows significant amounts of breast artery calcification (BAC), may identify a woman at risk of coronary arterial calcification (CAC) which is an early sign of atherosclerotic cardiovascular disease (ASCVD).
Substantial breast artery calcification should trigger a conversation about heart health
The authors of the recent studies linking breast artery calcification to coronary artery calcification and coronary artery disease are united in suggesting that the association they have uncovered should cause the creation of a new BI-RADS category. The reporting radiologist needs a way to tell both the patient and the treating doctor about the patient’s BAC status.
If that status includes significant calcification within the patient’s breast arteries, the medical team should be alerted for further investigation of the patient’s coronary arteries.
Coronary artery calcification treatment
That additional investigation might lead to the prescription of statins, to control the buildup of plaque, as well as lifestyle modifications that could intervene in time to prevent heart failure or heart attack.
It sounds simple, and it is. After all, in the scenario envisioned by the researchers, the mammogram has already been taken, and the breast calcification is readily ascertainable by the radiologist.
So the cost of the MRI will not need to be increased. Neither will radiation from the MRI need to be increased. In other words, there is nothing to lose by adopting a regimen of reporting calcification status. On the other hand, there’s a great deal to be gained. Such as lives poised in the balance.
About Dr. Aliabadi
As one of the nation’s leading OB/GYN’s, Dr. Thaïs Aliabadi offers the very best in obstetrics and gynecology, including telehealth appointments. Together with her warm professional team, Dr. Aliabadi supports women through all phases of life. She creates a special one-on-one relationship between patient and doctor.
We invite you to establish care with Dr. Aliabadi. Please click here to make an appointment or call us at (844) 863-6700.
We take our patients’ safety very seriously. Our facility’s Covid-19 patient safety procedures exceed all CDC and World Health Organization recommendations. Masks are required in our office at all times during the coronavirus pandemic.
The practice of Dr. Thais Aliabadi and the Outpatient Hysterectomy Center are conveniently located for patients throughout Southern California and the Los Angeles area. We are near Beverly Hills, West Hollywood, Santa Monica, West Los Angeles, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles.















