What is Placenta Abnormalities?
Normal development of the placenta during pregnancy is essential for an uneventful delivery. The placenta and its health are vital to the health of a woman’s pregnancy and fetal development.
The placenta is the organ that develops during pregnancy to nourish the baby. It grows inside the uterine wall, connecting to the baby through the umbilical cord. The fetal side of the placenta is called the chorionic plate, and the maternal side is called the basal plate. Throughout your pregnancy, the placenta is responsible for getting nutrients and oxygen into your baby’s bloodstream, as well as removing its waste products. Placental insufficiencies, intrauterine growth restrictions, and other placental conditions can cause issues for both mother and infant.
In rare cases, a pregnancy might take on some additional risks due to placenta abnormalities.

Risk Factors for Placenta Abnormalities Include:
- Ethnicity
- High blood pressure
- Multiple gestation pregnancy
- History of uterine surgery
- History of placental problems
- Maternal drug use
- Trauma to the abdominal
- High maternal age
- Maternal blood-clotting disorders
- History of smoking
Placenta Previa
The placenta grows from the point at which the fertilized egg implants in the uterus. Normally, this happens on the inside wall or ceiling of the uterus. In a condition called placenta previa, the placenta grows from the lower side of the uterus. The placenta then grows to cover the cervix, causing problems for delivery.
Studies in placental pathology suggest a placental attachment to the anterior wall is associated with shorter gestational age, low birth weight, lower Apgar score, higher prenatal bleeding rate, increased postpartum hemorrhage, longer duration of hospitalization, and higher blood transfusion and hysterectomy rates compared to cases with lateral/posterior wall placenta.
Placenta previa is a major cause of third-trimester bleeding and has been associated with severe maternal morbidity, including hemorrhage requiring a blood transfusion, disseminated intravascular coagulation, and possibly, emergency hysterectomy.
Symptoms and diagnosis
Placenta previa is often diagnosed in the third trimester, following an occurrence of bright red vaginal bleeding. The bleeding can be heavy or light, and it usually stops on its own, only to return again within a few days or weeks. Most women don’t experience any pain.
If the placenta is found to be low-lying at the routine second-trimester ultrasound examination, further evaluation for placental cord insertion should be performed.
Your OB-GYN can diagnose placenta previa with a routine ultrasound during a prenatal appointment.
Placenta Previa Complications
Placenta previa can cause severe, even life-threatening bleeding during labor, vaginal birth, or even immediately after delivery. In some cases, there is an increased risk of preterm birth and/or Cesarean delivery.
Treatment
Your doctor will evaluate the severity of your condition and make a recommendation based on your individual case. For mild bleeding, your doctor will likely recommend bed rest and advise you to avoid both sex and exercise. For heavier bleeding, you may need to remain on strict bed rest in the hospital.
Placenta Accreta, Increta, and Percreta
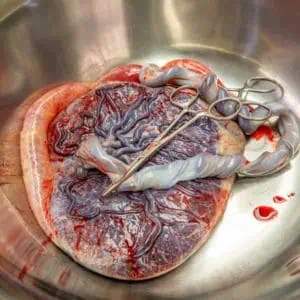
Normally, the placenta easily detaches from the uterine wall so that it can be expelled after the baby is born. This is known as the “afterbirth.” However, in rare cases, the placenta remains attached because its blood vessels, chorionic villi, have grown too deeply into the uterine wall but does not penetrate uterine serosa. This is called placenta accreta.
Placenta accreta can worsen if the blood vessels have impacted into the uterine muscles (called placenta increta) or if they have penetrated through the walls of the uterus (placenta percreta). In some cases in which there is a total invasion of the myometrium (placenta percreta) one can see the placental tissue protruding through the uterine surface. A thick ring of membranes on the fetal surface of the placenta may represent a circumvallate placenta, which is associated with premature delivery, prenatal bleeding, abruption, multiparity, and early fluid loss.
Circumvallate placenta is associated with poor pregnancy outcomes due to increased risk of vaginal bleeding beginning in the first trimester, premature rupture of the membranes.
The incidence of placenta accreta increases in women with previous cesarean delivery, other uterine surgery, advanced maternal age, high gravidity, multiparity, previous curettage, and placenta previa.
There is a risk of vaginal bleeding at the beginning of the first trimester and also pregnancy complications such as a risk of premature rupture of the membranes, preterm delivery, placental insufficiency, and placental abruption. The pregnancy outcome can be very poor.
Symptoms and diagnosis
Placenta previa, accrete, and percreta typically have no outward symptoms. Your doctor can catch the condition during a regular ultrasound, MRI, or blood test. Complications of this condition can include third trimester vaginal bleeding, severe postpartum hemorrhage, cesarean delivery, and subsequent hysterectomy.
Risks
Placenta previa and its variants can cause excessive blood loss after birth. Your blood may have difficulty clotting normally, and this could lead to lung and kidney failure. Placenta previa also increases the risk of preterm labor and premature birth. The highest risk for a placenta accreta is in pregnancies with a history of a cesarean section and a current placenta previa.
Risk factors for developing placenta accreta are mainly unknown. They are thought to include a history of placenta previa and previous cesarean sections.
Treatment
Treating severe blood loss in labor usually involves a blood transfusion. When the outcome is difficult to control, your health care doctor may recommend an early delivery to try to prevent you from going into labor naturally.
Vasa Previa
Vasa Previa is a complication in which fetal blood vessels, either in the placenta or in the umbilical cord, are trapped between the baby and the cervix. This can happen in a number of ways. One of the most common is when the placenta develops a minor (succenturiate) lobe, joined to the main placental disc only by threads of blood vessels, which cross the cervical opening. In cases of the bilobed placenta, there is no increased risk of fetal anomalies. However, this type of placental abnormality can be associated with first-trimester bleeding, polyhydramnios, placental abruption, and retained placenta.
In cases of vasa previa, velamentous cord insertion has been associated with low birth weight and an abnormal intrapartum fetal heart rate pattern.
Symptoms and diagnosis
There are usually no symptoms to signal vasa previa, but the condition can be detected with a sonogram and a Doppler ultrasound after the 16th week.
Pregnant women with vasa previa sometimes have painless vaginal bleeding in the second or third trimester. A pregnant woman who experiences vaginal bleeding should always report it to her health care provider so that the cause can be determined and any necessary steps taken to protect the baby.
Risks
Vesa previa typically causes no problems for either the mother or baby until the water breaks. This can tear the blood vessels, resulting in the baby losing a life-threatening amount of blood.
A pregnant woman may be at increased risk for vasa previa if she:
- Has a velamentous insertion of the cord (the umbilical cord inserts abnormally into the fetal membranes instead of the center of the placenta)
- Has placenta previa (a low-lying placenta that covers part or all of the cervix) or certain other placental abnormalities
- Is expecting more than one baby
Vasa Previa Management
To prevent a fatal outcome for the baby, it is crucially important to detect vasa previa before going into labor. When vasa previa is diagnosed by ultrasound earlier in pregnancy, fetal deaths generally can be prevented by delivering the baby by cesarean section at about 35 weeks of gestation.
There are suggestions that color Doppler ultrasound can be used to visualize the blood vessels in high-risk cases and, if required, elective cesarean performed at 35–36 weeks in cases diagnosed as vasa previa.
Rare Placental Abnormalities
Placental infarcts are areas of dead tissue found within the placenta, typically caused by blood vessel complications.
This placental abnormality decreases blood flow to the affected areas. At times, this can cause fetal growth restriction or death. Placental infarcts are more commonly experienced by women with severe high blood pressure.
An extremely thin placenta may represent placenta membranacea. In this condition, the entire uterine cavity is lined with the thin placenta. Placenta membranacea is associated with a very poor fetal outcome.
Leading the Way in Women’s Health – Dr. Thaïs Aliabadi
Recognized as one of the nation’s top OB/GYNs, Dr. Thaïs Aliabadi combines world-class expertise with a deep commitment to personalized, compassionate care. With decades of experience and a dedication to truly listening to every patient, she ensures that every woman who walks through her doors feels heard, supported, and empowered in her health journey.
We invite you to establish care with Dr. Aliabadi. Please make an appointment online or call us at (844) 863-6700.
The practice of Dr. Thais Aliabadi and the Outpatient Hysterectomy Center is conveniently located for patients throughout Southern California and the Los Angeles area. We are near Beverly Hills, West Hollywood, Santa Monica, West Los Angeles, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles.
















