What is an IUD?
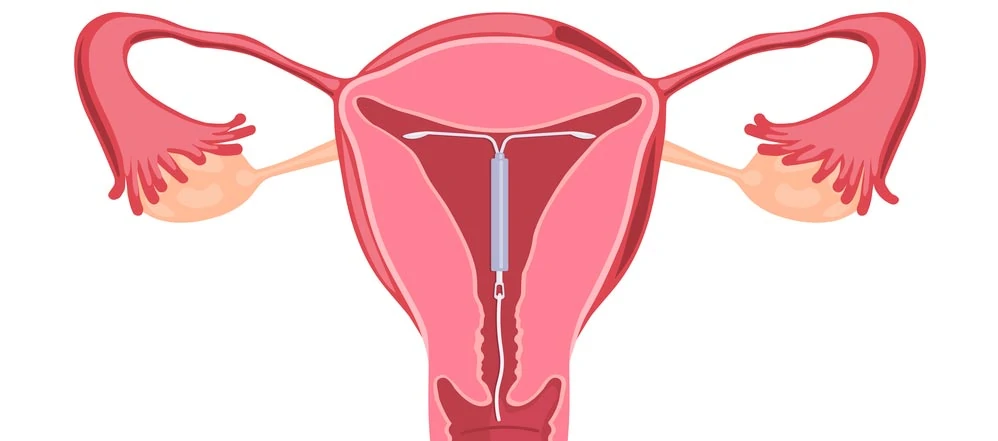
An Intrauterine Devices (IUD) is a form of long-acting, reversible contraception that is inserted and remains inside your uterus while preventing fertilization. The IUD is a small, T-shaped device about the size of a large paperclip. There are two types of IUDs currently on the market: hormonal and non-hormonal copper. Both must be inserted by a health care provider, and both are a highly effective method of preventing pregnancy for several years.
IUDs are known as long-acting reversible contraception (LARCs) because they can be used to prevent pregnancy for a long duration. The IUD and the implant are the most effective forms of reversible birth control available. During the first year of use, fewer than 1 in 100 women using an IUD or implant will get pregnant. Over time, LARC methods are 20 times more effective than birth control pills, the patch, or the ring. IUDs have been used in by American women for decades.
What is a Hormonal IUD?
The hormonal IUD is better known by its brand names Mirena, Skyla, and Kyleena. Slowly and over a long period of time, hormonal IUDs release levonorgestrel, related to hormone progestin. The hormone thickens the cervical mucus, which stops sperm from entering the uterus. It also makes it difficult for a fertilized egg to implant in the endometrium. Progestin also thins the lining of the uterus. In the unlikely event that sperm can travel to the egg, this thin lining makes it difficult for an egg to implant in the uterus and cause a pregnancy.
Mirena, Skyla, and Kyleena can all prevent pregnancy. Mirena can remain in your uterus for up to 5 years, whereas Skyla can only be used up to 3 years, but it is smaller in size and releases fewer hormones. Kyleena (which was FDA-approved in 2016) offers the best of both worlds, smaller in size, fewer hormones and approved for up to 5 years.
In most patients, hormonal IUDs can ease cramping and decrease menstrual bleeding.
What is a Copper IUD?
ParaGard is the most common brand of non-hormonal copper IUD. Wound around the stem of the IUD is a thin wire made of copper. The ParaGard IUD uses copper to prevent pregnancy. Sperm doesn’t like copper, so the ParaGard IUD makes it almost impossible for sperm to get to the egg.
Although the copper IUD is only a slightly less effective contraceptive than Mirena, it can remain in place for up to 10 years.
A copper IUD can be used as emergency contraception in some cases. If you’ve had unprotected sex in the past 72 hours and wish to continue using an IUD after insertion, the copper IUD can prevent a possible pregnancy. However, this option is more expensive than the oral Plan B pill.
How is an IUD placed in a woman?
You can make an insertion appointment with your Obstetrics and Gynecology at any time, as long as your pelvis is generally healthy, and you aren’t pregnant. Before insertion, your health care doctor may want to have you screened for STIs.
On the day of insertion, your doctor can prescribe medication to soften the cervix or administer a local anesthetic to help with the discomfort. The insertion can also be performed without drugs if you prefer.
The procedure is no more invasive than a Pap smear and takes less than 5 minutes. Some patients find the insertion painful, while others report that it feels similar to a menstrual cramp. The process tends to be easier for patients who have given birth vaginally in the past.
When your IUD is in place, you should be able to feel a small string hanging from your cervix. Your doctor can show you how to locate it. The string will not be visible from the outside and won’t interfere with sex. If the string is a little too long, your doctor can clip it for you.
What happens right after you get an IUD?
It’s a good idea to have a trusted friend or family member drive you home after your procedure. Most patients will experience some cramping and bleeding for a couple of days. Avoid inserting anything into your vagina during this time, including tampons, and avoid penetrative sex.
You may take ibuprofen and use a heating pad to manage the pain during the first day. You may want to take the day off work to rest. You should be able to return to work the next day.
IUD Follow-Up Care
Your doctor may schedule another appointment with you 3-6 weeks after your insertion. She will check to make sure the IUD is still in place and can address any questions or concerns you may have.After your next few periods, you should check with your fingers to make sure you can feel the string. It’s very uncommon for a patient’s uterus to expel the IUD spontaneously, but it can happen. Insert your finger into your vagina and feel for the plastic string. It will feel a little like fishing line.
If you can’t feel it, call your doctor. It may have been expelled, or the string may have just wrapped itself around the cervix. If you’re not sure the IUD is in place, use another form of contraception until you can see your doctor.
Who is a Good Candidate for an IUD?
An IUD is a safe, effective, convenient, and easily reversible form of birth control. An IUD may be right for you if you:
- Are in a low-risk category for STIs and pelvic inflammatory disease.
- Have only one sex partner who is infection-free.
- Use another form of contraception to guard against STIs, such as condoms.
- Cannot or do not want to use hormonal birth control methods.
- Find it difficult to take oral contraceptives daily.
- Are breastfeeding.
- Have a history of irregular bleeding, painful periods, or endometriosis.
Benefits of an IUD
- Extremely effective at preventing pregnancy. Less than 1% of women will become pregnant in the first year after insertion. Pregnancy is most likely to occur if the IUD has been expelled from the uterus without the patient noticing.
- Cost-effective over time. IUDs are usually covered by insurance plans, and provide contraception for several years after insertion.
- Easily reversible. If you wish to become pregnant, you can have your IUD removed by your doctor at any time.
- Easy to use. Aside from checking that the IUD remains in place every month or so, you can forget it’s there. You do not need to interrupt sex in order to protect against pregnancy.
- Significantly reduces menstrual bleeding and cramps after 3-4 months (Mirena). In some cases, periods may stop completely. This will not affect future fertility should you decide to remove the IUD to become pregnant.
- May reduce the risk of endometrial hyperplasia, endometrial cancer, and ectopic pregnancy.
- May treat the symptoms of endometriosis.
- Will not cause weight gain.
What are the Risks of an IUD?
- May increase cramps and menstrual bleeding (Paraguard).
- Increased risk of benign (noncancerous) ovarian cysts (Mirena). These tend to resolve on their own.
- Side effects such as mood swings, acne, headaches, and tenderness in the breasts (Mirena). These side effects tend to disappear after 3-4 months.
- No protection against STIs.
- Some patients may experience light spotting between their periods.
- Expulsion from the uterus. In 2-10% of cases, the IUD may be spontaneously expelled from the uterus during the first year. It’s more common in the early months after insertion, if the woman has never been pregnant, or if the IUD was inserted immediately after giving birth. The IUD can be re-inserted, but another form of contraception must be used in the meantime.
- Uterine perforation. In one out of 1,000 patients, the device may perforate (puncture) the uterine wall. This is a serious complication and will require immediate medical intervention.
IUD warning signs
Chances are that you’ll have no problems with your IUD. But it’s still important to pay attention to your body and how you feel after you get your IUD. Here are the warning signs to watch out for. Call your nurse or doctor right away if:
- the length of your IUD string feels shorter or longer than it was
- you can feel the hard-plastic bottom of the IUD coming out through your cervix
- you think you might be pregnant
- you have bad cramping, pain, or soreness in your lower belly or stomach
- there’s pain or bleeding during sex
- you get unexplained fever, chills, or have trouble breathing
- your vaginal discharge is different than normal
- you have vaginal bleeding that is heavier than usual
If you have unprotected sex with someone who has an STD, see your nurse or doctor for any tests or treatments you may need.
Do Intrauterine Devices (IUDs) Increase the Risk of Pelvic Inflammatory Disease?
No. This rumor began with a kernel of truth. If you have a genital infection when your IUD is inserted, there is a possibility that the infection can be carried to your uterus and fallopian tubes. To reduce this risk, your doctor will have you tested for STIs and treat any infection prior to IUD insertion.
However, hormonal IUDs may not be suitable for people with pelvic infections, uterine distortions, unexplained vaginal bleeding, and cervical or endometrial cancer. They also do not protect against HIV and other sexually transmitted infections.
Concerns about your IUD? When to Call Your Doctor
Call your doctor right away if you:
- Experience heavy vaginal bleeding, such as if you have soaked through a pad or tampon each hour for more than 2 hours.
- Experience severe pelvic pain.
- Have a fever or chills.
- Notice foul-smelling vaginal discharge.
- Cannot locate the string of your IUD, or if the string feels longer or shorter than usual.
- Might be pregnant.
- Might have contracted an STI.
What if I Become Pregnant with my IUD?
If your Intrauterine Devices (IUD) becomes dislodged from your uterus, there is a chance you could become pregnant. In this unlikely event, your doctor will recommend that you have the IUD removed, as it may cause miscarriage, ectopic pregnancy, or preterm delivery. The IUD will not increase the risk of birth defects
About Dr. Thaïs Aliabadi
As one of the nation’s leading OB-GYNs, Dr. Thaïs Aliabadi offers the very best in gynecological and obstetric care. Together with her warm professional team, Dr. Aliabadi supports women through all phases of life. She fosters a special one-on-one relationship between patient and doctor.
We invite you to establish care with Dr. Aliabadi. Please click here to make an appointment or call us at (844) 863-6700.